Show Notes
- Heidelberg Test – Ask your doctor
- Microbiome Test – Order one to take at home, at your leisure
If you are new to this site, you should first read my How I Cured My Silent Reflux article as it explains the underlying root causes of acid reflux, its corresponding treatments, and provides the necessary context to follow some of the concepts in this episode.
Episode Transcript
(Note this is not a word-for-word transcription - it's loosely paraphrased. Alternatively, feel free to watch on YouTube).
Challenge of Traditional Acid Reflux Medicine
So the gap between what I thought my acid reflux appointments would be like and what they were actually like was pretty big. And that left me eventually realizing I was gonna have to kind of go in on my own. But the challenge is there is a lot of information out there and how do you know what’s good and what’s bad? And that’s a lot of what I hope to accomplish in the video today is kind of talk you guys through not just more noise than I’m adding to the pile, but instead more of the actual science. And so you will be in a better position to have a meaningful dialogue with your doctor, but also be in a better position to understand some of the things that are out there in the holistic healing space and be able to test and approve those things for yourself. So why don’t we go ahead and jump in?
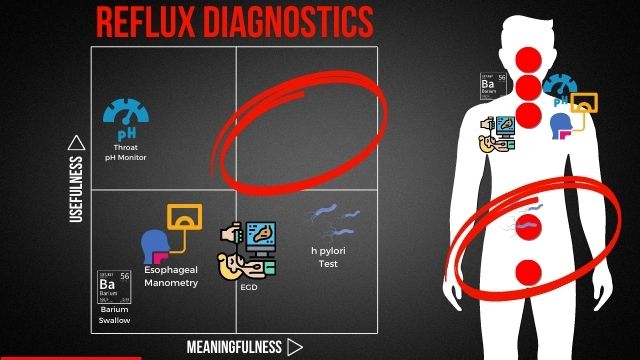
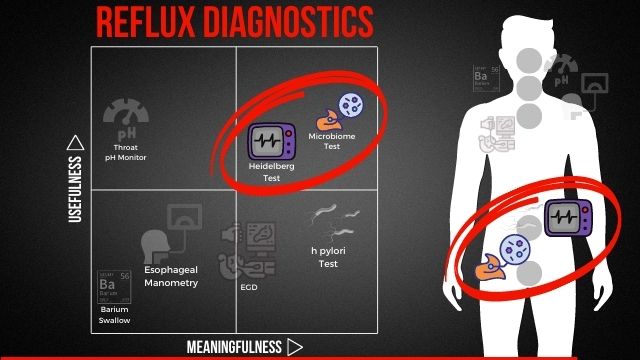
For me, I think one of the biggest opportunities with all of us coming together here is really to build a sense of community and to be able to sort of lift each other up with constructive information. I know a ton because I’ve been able to heal my reflux through holistic methods, through a lot of research that I’ve done, up until that point, and everything that I’ve done after that, but I don’t know for sure, as much as we all do collectively. So I would love for us to be able to really dig in and share as much as we possibly can to help each other kind of grow and learn. This chart that I’ve got here on the YouTube screen, you may recognize. So if you look at the bottom left-hand corner, some of you may have seen that before, and if you have, let us know where. The one on the right is new, but what I wanted to do is for you to get some eyeballs on that and identify what maybe is interesting about it. And go ahead and drop that into the chat.
So one of the things you may notice in this chart here, and I’ll kind of talk you through in a second, is that there is kind of a big chunk missing in the top right-hand corner. If I were to describe the chart, for those of you that may not be able to see it, there’s four quadrants to it. In the bottom left, you’ve got the items that I would consider to be more useful and more meaningful, and in the top right, it would be the ones that would be the most useful and the most meaningful. This is a chart of my own making, and what I’ve done is I’ve taken all the popular reflux diagnostics, and I’ve sort of thrown them up on a chart.
E.G.D. Diagnostic for Acid Reflux
And you may wonder, you know, why would I say an E.G.D. is not very useful. I’ve had an E.G.D., and I would guess that many of you have had them as well. And essentially what it does is it takes a camera, sticks it on the end of a tube, and you’re able to drop that in through your mouth, and there we’ll do a visual inspection of your esophagus, your lower esophageal sphincter, and down into your stomach. And what that allows you to do is to get a pretty quick read-on, any sort of visual indications of issues with your digestive tract.
So why would I consider this to be not very useful? Well, the E.G.D., for one, you typically will go into the office, see your doctor, because you feel like you’ve got acid reflux. It’s one of those diseases that I think is pretty well known. We can all sort of self-diagnose that. So when you get into the office, they’re gonna do this E.G.D. test, and they’re gonna try to confirm that. Usually we don’t really need a confirmation of that.
In addition, if it doesn’t identify any sort of significant issues, like inflammation in the throat in the case of Barrett’s Esophagus or esophagitis, or inflammation in the gut or ulcers in the gut in the form of like gastritis or ulcers, the diagnostic itself is not particularly useful. And I feel the same way for some of these other diagnostics as well. So the pH thermometer, as an example, it will check the pH levels in your throat, and so if you do have any reflux events, it will detect that. But again, it’s sort of confirming reflux, but not providing any additional information. I would expect a diagnostic, if it was gonna be used by a doctor, to actually provide additional information for them to provide more advanced treatments. But I think, as many of you probably know, the treatments are gonna end up being the same.
Esophageal Manometry for Acid Reflux
But I feel that way for a lot of these diagnostics. The esophageal manometry is really about trying to understand the motility in your throat. Typically, when you’ve got any sort of absolute reflux issues, other things that go along with it will cause you to have issues with moving food along your digestive tract. We’ll talk a little bit more about that as we get into the subsequent charts, but it’s sort of a given that you’re gonna have some level of motility issues. Barium swallow just gives you a higher resolution x-ray.
H. Pylori Test for Acid Reflux
On this chart though, the one that I would find to be slightly more meaningful, but still not that useful, would be the H. pylori test. Why is that? If you actually look at the world’s population, about 50% of people in the world actually have H. pylori present. It’s not bad in and of itself, and in fact, some studies have shown that H. pylori participate in the digestive process in a beneficial way. But it’s when the bacteria is able to overgrow that you will actually run into some issues. And so I’ve done H. pylori tests. There’s like four different ways you can do it. You can do a breath test, you can do a blood test, you can do a stool test.
But basically, if you’ve got an overgrowth of H. pylori, you’ve got problems. If you don’t, probably to the levels that it wouldn’t be detected on these tests, it’s not particularly useful as well. My real challenge with it though is that they do this singular diagnostic for this one strain of bacteria. And we’ll talk more about this, but I think many of you understand that there are other strains of bacterial overgrowth that can be a challenge. I think a broader look at this would be much more useful.
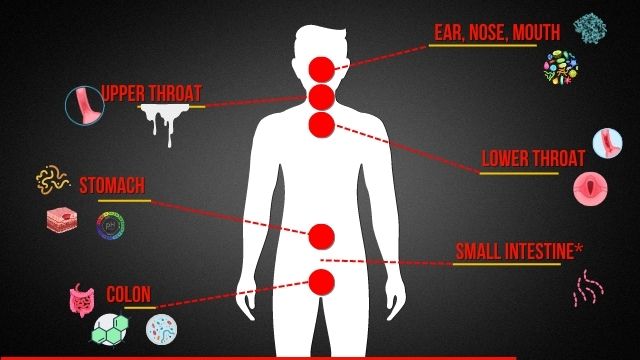
So one of the things that really stood out for me as I was putting these materials together is that a lot of these diagnostics are really centered around the top portion of the body. And you might ask yourself, why is that? Well, years ago, as people were kind of diagnosing reflux, a lot of the symptoms are occurring up here, right? You’ve got some acid that you can feel in your throat, sometimes it can get into your mouth. And so it makes sense for those diagnostics to kind of start there. But fast forward decades, you would expect that as our understanding of the disease grew, that our diagnostics would have expanded as well. And that’s just not really the case. So a lot of those diagnostics are centered around the throat area, which is kind of in the symptom management space.
That’s not really in the deal with the issue space. And we’ll talk a little bit more about that. But in general, as you move down, that adjusted track, you’re gonna start to get into the areas where you can do something about your reflux as opposed to mitigating symptoms. And that’s the other kind of overriding broad issue that I have with the diagnostics you get in the sort of mainstream medical field. So I think there’s something missing here in this top right and lower down where there’s something meaningful that can be done.
So I do need to mention to you all that I am not a doctor, not a naturopath, I’m not a functional medicine provider. I’m nothing. I’m just a guy who was able to heal his acid reflux after 15 years of struggling with it. And it got to a point where it was so bad that I had no choice but to look for alternatives.
There were a lot of research, reading through medical journals and things along those lines. I was able to heal my reflux. And in doing so, I realized that there’s gotta be so many other people like me. With 20% of the US population dealing with some form of reflux on a weekly basis, I just knew I had to get this information out in a much more digestible form. So I say all that to say, I’m not a doctor. I don’t know your particular situation. And so this is not medical advice. These are things for you to consider with your doctor and for you to consider if you’re thinking about a care for yourself.
One of the other things, as you contrast traditional medicine approach to modern science approach and going back all those years, as I mentioned about how some of the medical establishments got set up is they tend to think about the human body still as a bit of a machine. So with a machine, if you’ve got it faulty part, you can pull that piece out, put in a new piece, maybe loop something up and then it’s ready to go. And that simplistic way of thinking about the human body was probably fine, you know, 50, 100 years ago. But nowadays that kind of breaks down. I think modern science would recognize that we’ve got a much more analogous situation to a distributed computer network. And for any of you that are not technical and you’ve tried to solve a technical issue, you know that that can be difficult. Like is it an issue with the server? Is it an issue with the software? Is it an issue with the data that I put in? And troubleshooting that requires a more holistic understanding. Yet the traditional medicine space is still stuck with this. Okay, if you’ve got an issue with your, the top part of your body, you go to an ear, nose and throat doctor. Or if you’ve got an issue with your stomach, maybe go to a gastroenterologist or you go to a heart surgery or brain surgery. I get it, it’s complex. But what that doesn’t allow those practitioners to do is think holistically.
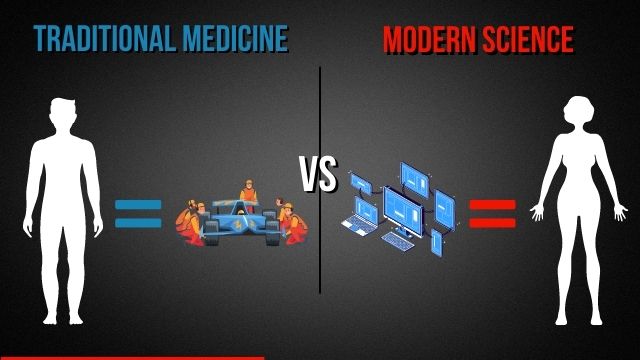
And I’m really curious how many of you, and just let me know in the chat here, have gone to an ear, nose and throat doctor as opposed to a gastroenterologist for your reflux. And I think we all intuitively understand that this is a digestive disease, not really an issue with the ear, nose and throat. Just let me know in the comments where you’ve gone. I was sent to an ENT for my E.G.D. which makes sense. They do the procedure through the mouth. But are they in the best position to really help me with my reflux? Probably not, right?
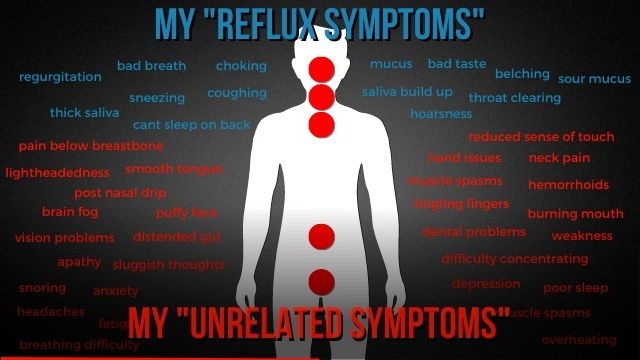
Okay. You know, if I were to look at some of the symptoms that I feel comfortable talking to my doctor about, and you guys tell me if you’ve had this experience as well, I can talk to my doctor all day about the symptoms here in blue. And in fact, these are all of my symptoms over the 15 years that I dealt with this. I put it together, I realized this is a ridiculous list. But if I start talking to my primary care physician, my ENT about some of the stuff in red, they start to give me funny looks and they start saying, you know, some of this maybe is in your head, this is unrelated.
I see some comments here from Deborah, “I’ve been to ENT, a GI and a pulmonary”, that’s great. So it sounds like your doctor maybe is having you look at a few different specialists.
John says “ENT and GIs, ENT now going to a GI doc”. Chris Chateau has gone to ENT. So they got a little bit of a mixed bag here and that comes back to a lot of the specialists and a lot of the primary care physicians kind of work within their lane. And it’s not really easy for them to kind of understand what are the practitioners they want to, may want to bring in in order to give you a more holistic diagnostic.
Yeah, so comment from Craft Crush, you know, that’s a really common one about having allergies and indications and being diagnosed with a bias specialist. When I went in with some of my more severe versions of acid reflux, solid reflux, they gave me a, what do you call it? Sleep apnea test and they gave me a H. pylori test because they really didn’t know what was going on with me.
So this is a bit cliché, but kind of think about everything that I’ve talked about before, sort of the hyper specialization of the traditional medicine approach, the fact that the diagnostics are kind of in the symptom management space. There’s not really a holistic understanding of all the symptoms and how they may interrelate or even where you would go to solve these issues. Furthermore, they wouldn’t know where to send you because everybody kind of has their specialty in the body.
It kind of feels like a red pill, blue pill situation, right? You got the blue pill here on this one side and then, you know, after you’ve gone through that and kind of run the gambit, you may start to look over here on the right. Now for me, I grew up in a medical household. I spent upwards of 40 years at the dinner table hearing about medical things. My dad’s a doctor. And so I was firmly in the blue pill space. I used to laugh at people that talked about, you know, holistic stuff, don’t talk to me about essential oils, organic food, any of that stuff, right?
But when my health got real bad, suddenly the red pill looked really interesting. And I gotta tell you, there’s a lot to offer in this space. So last thing I’ll say about the traditional medicine piece, and guys, feel free to ask any questions, anything that’s unclear. Traditional medicine is typically just going to look into areas. One is gonna be kind of in the throat region with all the diagnostics that we shared on the prior slide.
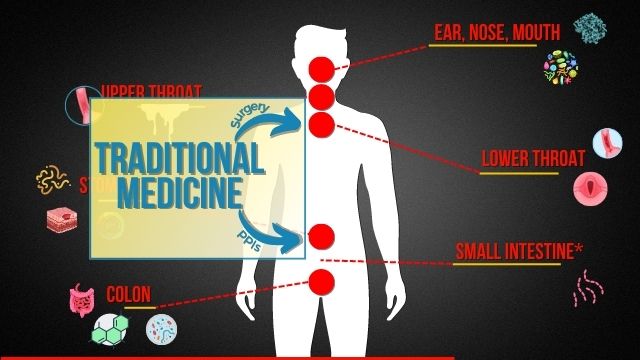
That may offer PPIs that will mitigate the acid that will get to that region, or they may offer surgery. But if you think about both of those, surgery is going to put a band-aid on the situation without dealing with everything else that’s going on. And so what do you think is gonna happen in five, 10, or 15 years as the rest of those symptoms continue to escalate or bubble over? That’s why a lot of the surgeries, if you look at the clinical results, don’t have a long track record. Or PPIs, which come with a whole host of other issues that we’ll talk about as we kind of go into this next slide a little bit.
Deborah, thank you for commenting. So “Dr. Jamie Kaufman thinks along the same lines as you do.” The issue has to be looked at more broadly, and it’s not just the GI space under the umbrella as good. You’re absolutely right. When I was doing some of my initial research, I ran across a lot of her stuff. She coined the term silent reflux, which was pivotal for me, because had she not, I may not have had enough descriptive language to do the research that I need to figure out how to deal with my issue, or even to realize a lot of these symptoms were sort of related. So I’m certainly very thankful to Jamie Kaufman. And I think this is why I’m so excited about bringing this group together, across all the different platforms that we’re on, well over 10,000 of us. I think each one of us has got a little bit of pieces of information that I would love for us to be able to kind of coalesce and be able to help each other accelerate our healing journey much faster. So thank you, Deborah, for jumping in with that comment.
So let’s talk a little bit about each of the five areas. This is the reason that you’re all up here. I think it’s critically important to understand the actual science that’s behind some of the challenges that we deal with when it comes to reflux. Because without that solid understanding, you get blown in the wind by the doctors. They’re doing their best. I’m not trying to throw shade at them.
But they’ve got a limited tool set for the pharmaceuticals. They’ve got a limited tool set from, you know, all the diagnostic machines. And they’ve got limited time. And this is one of umpteen number of diseases that they need to be able to understand.
So I’m not trying to throw shade, as I said. But that means that even for a disease that seems as routine as acid reflux is, you’re gonna probably have to go it alone. And this is why a lot of you are kind of with us.
So Craft Crush says, “Unfortunately, I’m in PPIs again, “because when I try to the holistic doctor, “the results were horrible. “Maybe unlucky with somebody who’s not that good.” It could be Craft Crush. And you know, the more you educate yourself with this stuff, the more you stick with this channel, you can understand that science to the point where you can really have that detailed conversation. Test the knowledge. I think, you know, if you watch a few of my videos, and some of them get really deep, I’m gonna try to make them a little bit more packageable in the future.
You’ll see pretty quickly that if you go have a conversation with your doctor, and many of you have done this, you’ll find that you’ve surpassed the knowledge really quick, and you realize, okay, maybe this person is not in the best position to help me. And that’s what I hope to do for you all. So you can figure out, is this the right person for me? And maybe shop around before you have the bad experience. I’m sorry for that.
Okay, so let’s start with the ear, nose, and mouth. Now keep in mind, as we go down the gastrointestinal tract, you’ll begin to be more in a range where you can do something to start to address some of the underlying issues with reflux. Even as we talk about the stuff that’s sort of above the stomach line, you’re starting to get into sort of symptom management. Maybe take the edge off of some of the symptoms, but maybe not necessarily deal with the symptoms directly.
Aloe Vera for Acid Reflux
Shannon, thanks for sharing. Fresh aloe vera has been helping a little bit. How often do you recommend having it? I actually have not done a lot of research on fresh aloe vera, and I’ll be very forthright with you on anything that I do share. It’s because I’ve had personal experience or because I’ve extensively researched it. I’ve got in mind to research a lot of these other herbal remedies. In fact, I’ll be posting to Instagram shortly, what would you guys like to see in this next video? And I have aloe vera on the list of five other herbal remedies that you guys can consider if you wanna see that next. So I don’t wanna offer any suggestions beyond recognizing that it is something that is oftentimes recommended for helping to improve some of the gut lining to provide a little bit of a cushion between what’s going on in your stomach and areas that may be compromised in the gut lining. Its effectiveness, I have not researched it yet, so I’m sorry, I can’t speak to that.
What are Pepsins
But when it comes to your nose and mouth, there’s really two big challenges. One, I really dealt with, which were pepsins. Pepsins are these little digestive enzymes that are in your stomach and in some situations, they can get into the soft tissues outside the stomach. So they can get into your throat, they can get into your mouth. For me, it was embedded deeply in the roof of my mouth, little spots on my tongue and also on my nose. It was excruciatingly painful.
But when they get there, you’re kind of in this mode of just trying to flush them out. There’s not a lot you can do if you haven’t stopped the underlying reflux issues to get them out other than to, you know, try to drink a lot of water. I drink a lot of warm water, get a lot of kind of brushing all surfaces of my mouth. Things like that to try to help the pepsins sort of move on. The other big thing is if you’re dealing with this situation, it’s a void like the plague, anything that has a high acidity. And you’re looking for foods that have a pH of five or less, so anything between five and one is gonna be acidic. The reason for that is pepsins are actually activated by acidity.
That’s why you wanna try to avoid those things. So it doesn’t, you know, this is not something you can do to sort of heal yourself from having to deal with pepsins. This is sort of the symptom mitigation. Again, above the stomach, that’s sort of where you are.
Oral Bacteria Acid Reflux
Bacteria actually gets really interesting, maybe in a bad way. Typically, you know, the flow of bacteria may be from your mouth into your stomach. You’re eating different things. You know, you may lick your fingers when you touch different things. And your body’s really designed to be able to handle those sort of things. So as a pathogen or bacteria gets into your stomach, the acidity in your stomach will typically burn that off. And if not, then your immune system kicks in.
In the case of reflux, you’re getting kind of a bidirectional flow. So some of the bacteria that’s in your stomach, in particular, in a low acidic environment, we’ll talk about why your low acidity may be the case for you, is now refluxing back into your mouth. You can get some pretty gnarly stuff going on in your mouth. And so dealing with the bacteria can be a challenge as well.
You know, there’s some dental probiotics that I’ve tried in the past. I’ve had sort of hit or miss success with those. The thing that had worked the best for me would be a non-alcohol-based mouthwash. And if you could use one that does not have alcohol in it, that seems to do the best. And with things like mouthwash, you really wanna not do it very often. It’s sort of like dropping napalm in your mouth. You wanna kind of maintain a homeostasis in your mouth if you can. But if you’ve got these reflux events that are introducing bacteria, and you’ve got sort of breath issues and other things that are going on, sometimes you have to kind of break it down.
Go back and look at some of the comments here that they have missed. So comment from mycliffe:
“So I followed the advice in your book, strict diet supplementing with HCL, my condition greatly improved, but it didn’t go away completely. Any advice how to finish the job?”
Yeah, depending on the state of dysbiosis that you may be dealing with, and dysbiosis is an imbalance of the microbes in your digestive tract. We’ll talk about that in a little bit more detail here in a second. Depending on how advanced that is, it may take you longer to sort of work through full restoration. You know, what I did after I kind of spent my first two months going through the program and felt really good,
I spent, you know, from there up until today, making sure that I’m trying to eat well in the base case. Now I indulge now, I enjoy, you know, snacks, desserts and that sort of thing, but I try to eat healthy in the base case because I know for me, the risk factors that got me into reflux in the first place were really poor diets. I don’t ever want to go back there again. So that means including a large degree of fiber in my meals, pretty much at all times if I can. If not, I try to make sure I get a good adjustment of fiber through the course of the day. And so, you know, it may take a little bit longer.
If you’ve been going a really long course, you may consider a gut biome test to give you sort of directional information if you’ve got significant imbalances in certain areas. This is an evolving science, it’s not perfect. I share on my website a link to a microbiome test that’s put out by a company called Biome Health, listening to some of the materials that are on the cutting science of what’s going on, you know, as new information becomes available, they’re gonna incorporate it into their test, but it’s not perfect. There’s a lot of different reasons if you want to hear more about why it’s not perfect. Happy to kind of go into that. But if you were to get one of those tests that’ll give you maybe a stronger sense of where you could maybe supplement with probiotics in addition to the fiber.
But if you’re seeing any additional symptoms, then it may be that you need to continue with some of the other supplements and things that we talk about in the book for a little bit longer. Pain-free coach,
“enzyme super helpful, probiotics, but mainly enzymes”
that’s great to hear. Thank you for sharing. Like we all grow and learn together, the more that we can share.
Gut Health Connection to Many Diseases
Hey John, thanks for the comments. So celiac and gluten sensitivity is definitely correlated with stubborn reflux as well. Yeah, you bring up a phenomenal point. You know, with the advance of microbiome science over the last 20 to 25 years, we’ve started to learn a lot of things. So things that we traditionally consider to be these big monolithic diseases like autoimmune disease, celiac disease, or some other ones, even diabetes, acid reflux, allergies, autism. All these are now being directly correlated to imbalances in the gut.
Right, so think about what that means. That means that diabetes is not the disease. Diabetes is a symptom of a gut health issue. Acid reflux, the more I learn, is not a disease. It’s a symptom of gut health issues. And so this is why you start to see this crossover of symptoms where you’re allergic to certain things, you never had allergies before, you’re kind of like, what’s going on here?
But also where as you start to resolve some of those things, kind of going back to my blue and red chart, a bunch of other stuff goes away that doesn’t seem to be acid reflux related. Thank you for sharing that, Joe. That’s a very, very critical point.
So Wellie360, appreciate your comments. So I had a chronic reflux after antibiotics cured with B-tain hydrochloride to replace my acid. Also fermented foods and milk. So it took a year to work it all out. That’s fantastic. So first of all, I’m super excited that you’ve been able to get back on your feet and get back to normal. Keep up the good work there because you can continue to build robustness in your gut. Cannot be more happy for you. But you bring up a number of good points there. Fermented foods, a great sources of prebiotics and B-tain hydrochloride is a really great tool we’ll kind of get into here in a second. Antibiotics, I neglected to mention that on the prior slide. So you’ll typically get hit with PBIs, surgery as an option.
Feel like you've done all the things and are just not seeing progress? I've helped a lot of people over the years that felt the same way. Perhaps an at home microbiome test can help break the cycle and provide the insights you need to move froward. With it, you can test your gut microbiome and receive actionable recommendations on how to optimize your digestive health with the BIOHM Gut Report.
I have arranged a 20% discount if you use the code THEACIDREFLUXGUY at checkout!
Antibiotics Make Acid Reflux Worse
But the fallback option is antibiotics. And sadly, antibiotics are thrown around when the doctor just doesn’t know them, just to give you something to get you to go away and support that with studies that point that out. Particularly in pediatrics, parents will come in with their little kids, something’s not right. They don’t know what’s right, but they know that the mother will be perfectly fine if they give them some antibiotics and send them home.
Antibiotics are one of the worst possible things you can ingest if you are not needing it. And not in severe cases, never take an antibiotic. And I can say that very, very confidently. So we’ll talk about in a second, it destroys your gut balance. There are narrow spectrum antibiotics and those are gonna be your best option. But man, you gotta make sure that your doctor is equipping you with things that will help to offset that. Or you’re gonna get yourself into some trouble. I can say at least half of you that reach out to me either are coming to me because antibiotics made your reflux worse or you developed reflux because of antibiotics. So stay away from that stuff.
Upper Throat and Acid Reflux
So the upper throat, this scenario where you can start to get into some of the inflammation, this is where like the E.G.D. can actually have some merit. We’ve got some scar tissue that’s going on due to the frequent presence of acids in your throat. This scenario where you can start to develop that mucus response, this is my second most infuriating symptom. I was the mucus that would come into my throat right after I ate, right after I drank anything, even if it was just water. It would just be the onslaught. And that’s because once my lower esophageal sphincter opened up, for me with silent reflux that aerosolized the acid vapors and they went up into my throat.
And then your body just tries to coat it with a little bit of mucus in order to avoid damage. But it’s not a perfect solution. As you continue to have that happen over time, you can start to develop some level of damage. What’s really interesting, the body is designed in quite an amazing way. Just above the lower throat, which we’re gonna talk about now, the body will start to replace those damaged cells with stomach cells because they’re a little bit more resilient. And you can start to see in the case of Barrett’s esophagus that many of those folks will have stomach lining going all the way up their esophagus.
Unfortunately, as that continues and continues to take damage, it can start to get into sort of the cancerous range and things along those lines. But your body really does a lot to try to fight some of the damage that can come with reflux. Okay, so lower throat, here’s where you can start to get into kind of that borderline in between symptom management and actually try to deal with something. Just don’t accept a management, but you’re starting to kind of cross over a little bit.
Lower Esophageal Sphincter
The junction between your throat and your stomach, some people refer to it as the diaphragm, other people would refer to it as a esophageal sphincter, which is a ring muscle, similar to kind of your posterior. It opens and closes. And this is the main thing that would keep things from refluxing out of your stomach, right? In the normal case. Well, in the case of an asymptomatic sufferer, there’s a lot of things going on. So for one, if you’ve got a lot of indigestion, a lot of gas build up, that’s gonna put upwards pressure on the esophageal sphincter muscle. And actually the weakest direction of closing strength is from the bottom. And so if you’ve got a lot of pressure, just continuing to process that, but got a lot of food in there, you got a lot of gas in there, or this happens all the time for you, it’s gonna lose closing strength and it can open up.
Also, if you’ve got a lot of acid hitting that area often, or if you’ve got a lot of acidity from your food and drink, this is another area where you can start to develop inflammation, it can start to deform a little bit because of swelling up, that will cause a loss in closing strength. One of the big challenges in the Western diet is the fact that we have a tremendous amount of background acidity in our food. Sodas, for one, highly acidic, but really all of our canned foods, all of our packaged foods, the FDA requires a certain amount of acidity in order to keep bacteria from overgrowing. And so when you ingest that and you’re healthy, it’s not a big deal. But if you’ve got a frequent exposure of reflux acid due to reflux, or you just eat it and consume a lot of acidic drinks and foods, it’s gonna be compromised, it’s gonna be inflamed, and it’s gonna cause you issues. Some people that are like super early on in their journey can get away with just avoiding all the acidic stuff and the reflux may even go away, particularly if they start eating well.
But as you advance, this is just one more complication on top of a bunch of other things that are going on down deep in your body. There are other foods that are known to relax the esophageal sphincter. You’ve probably heard things like teas and coffees that can cause the tone to relax and that will cause things to open up.
So one of the things you have most in your control is take a close look at the pH level of the foods that you’re ingesting. You see stuff online that talks about avoiding acidic food. It’s not really about your stomach, if they’re making sense with what they’re talking about. It’s not really about your stomach. In that case, it’s about avoiding additional inflammation in the esophageal sphincter, which is just one line of defense against reflux. Okay.
So Vapatching, Vapatching said,
“I successfully healed with your program.” It took me two to three months to be successful. To get off HCL, but got there in the end.” I just want to give followers hope that it may take longer than six weeks.
Great, congratulations. Yeah, it’s a really good point. Just to build on the one that we made earlier, it really depends on the extent of your gut dysbiosis. Ah, I wonder how we could know if we have low stomach acid or high stomach acid. I think you’ve cheated. You looked at the back of our presentation here.
High vs Low Stomach Acid
So if you were here for the beginning part, I had a four quadrant diagram where I had all the popular reflux diagnostics on them. And there was a big glaring hole in the top right-hand side, which would be diagnostics that I find to be useful and meaningful.
One of the ones that will be missing there would be exactly what you’re asking about. How can I know if I have low stomach acid or high stomach acid? A link to a video that you can check out to see this diagnostic induction will be in the show notes after this publishes. But the technique is called the Heidelberg test. Now it is a mainstream, well, I should qualify that. It is a traditional medicine diagnostic. However, it is not widely available. So you can ask your doctor for it. If you’re lucky, they’ll have it, but they may not.
But what it is, is you swallow a radio transmitter. It goes down into your stomach and they’ve got you hooked up to a monitor. And what they’ll do is they’ll have you drink a bicarbonate solution, which is basically an acid. And they measure your stomach pH or acidity when you very first ingest it. And then they measure how long it takes for your stomach to rebound after drinking that alkalenic drink. And based on the amount of time it takes to rebound, it’ll tell you your level of acidity. So you can find that you’ve got a high level of acidity based on the pH or a low level of acidity. Now, this test I find to be useful only in the sense that some people are sitting on the fence on whether they should take certain supplements.
This can help put their mind at ease that they do indeed have low stomach acid, if they do. A vanishingly small number of people in the world have high stomach acid. It’s a condition called hyperchlorhydria. I’ve met one person that’s got it in three years of talking to thousands of people. So it could be that other people didn’t mention it, or again, because the Heidelberg test isn’t available. But I think the vast majority of people that are dealing with reflux have low stomach acid, either because of vitamin deficiencies that come from a poor digestion or because they’re taking acid reflux medications, which by design lower your stomach acidity and compromise digestion. So I hope that helps answer your question.
So then if you get into the stomach. So now we’re starting to get into areas that matter when it comes to actually resolving some of the underlying issues with your acid reflux. I’ve been alluding to and talking a little bit about some of the imbalances that can occur. One of the very first areas where you can start to see imbalances occur is actually the stomach. But as you descend through the gastrointestinal tract from the mouth all the way down into the posterior area, you’re gonna have increasing prevalence of microbes that assist you with the digestion process. But that first core colony of it is gonna be in your stomach.
You probably have heard people say eating fiber is really important for maybe like bowel movement or something like that, to kind of get your regular. You may not know that human beings actually cannot digest fiber at all. Like not even a little bit. We are designed to have a symbiotic relationship with a host of and trillions of microorganisms that help to digest our food. And the beneficial variety of those actually thrive entirely on the fiber in your food.
Which is a big issue and why you can start to see why people in the Western hemisphere are starting to have issues with reflux. With about 20% of people having at least a couple of occasions of acid reflux throughout the course of their week. It’s because we just don’t eat enough vegetables or fruit. One of the things that sort of cracked me up and was also sad was when I took a cooler full of oranges to my son’s soccer game.
I handed them out to everybody. Some of the kids kind of looked at it like, what is this? And one kid even was like, I don’t know how to open this. And other kids were like, I don’t eat these. That’s a sad day. We’re at a point where kids, we know they don’t eat vegetables. I mean, that happened when I was a kid, but they don’t even eat fruit. And we are flushing our health down the tube really fast. Because the beneficial bacteria have to have fiber to live. And over time, those beneficial populations are gonna decline and here’s the issue with it.
At the base case, you can poorly digest your food. You might think, okay, we’ll have a little bit of indigestion. But it gets worse as you get farther down into the lower areas of the colon. The bacteria there that are participating in your digestion help you break down the foods, yes. But they also produce short-chain fatty acids, which are key to reducing inflammation in the body. They participate in and create hormones that your body uses to regulate mood, sleep, control the enteric nervous system, which is the conductor for your entire digestive system. So you can start to see pretty quickly that if you start to lose these beneficial bacteria, you’re gonna have a lot of problems.
And so, you know, the Western diet in the best case, when we’re eating healthy, looks like a big pile of meat with a couple of sides. We gotta reverse that. It’s gonna be a big pile of sides and a little bit of meat to start to get back into that sort of healthy range.
3 Types of Gut Bacteria
But anyway, so the stomach is kind of that first area where you do need to have a beneficial balance of bacteria. There are three types of bacteria in your stomach, in your colon. These are beneficial bacteria, commensal bacteria, which either don’t have a function or it’s not known. And I would say probably the most of us just not know to this point at this date of our science. And then you’ve got the pathogenic bacteria. Interestingly enough, beneficial bacteria can become pathogenic if they overgrow. So H. pylori is one of those that’s always implicated as an example in acid reflux.
It has a tendency to overgrow. When it does, it shifts from beneficial to pathogenic. But other bacteria, even some of the garden varieties, the ones that are provided in probiotics, if they overgrow, they can flip a switch and become pathogenic as well. And so keeping this balance is critical. You need all the good guys to help you with digestion. And to participate in all these other things. Thyroid function as an example is dependent on healthy gut microbiome.
But also in the stomach, in addition to some of the bacterial issues, you’re gonna start to see that some of the bacteria that help you with digestion actually live in the gut lining. So your body in this symbiotic relationship produces a gut lining that feeds some of the beneficial bacteria and then gets replenished. So it’s not a problem. But when you’ve got some of these imbalances, the bacteria can overgrow and is able to consume more of the gut lining than your stomach is able to replace.
 This is the probiotic gut reset program that I did after healing my acid reflux. Even so, I could feel the difference and improved resilience in my gut. I did 10 days of each probiotic in sequence. Be sure and ramp up your daily fiber intake to 35-50 grams daily to support the probiotics.
This is the probiotic gut reset program that I did after healing my acid reflux. Even so, I could feel the difference and improved resilience in my gut. I did 10 days of each probiotic in sequence. Be sure and ramp up your daily fiber intake to 35-50 grams daily to support the probiotics.
Leaky Gut
And then when your gut lining is thin, you start to get things like leaky gut, which I thought was a bit of a gimmick when I first started researching some of this stuff, because it’s kind of a weird thing. But it’s a real condition. You start to have lesions in your stomach where you’ve got thin gut lining and it allows food and bacteria to start to enter the bloodstream. And so this is when you start to have inflammation in all different parts of your body. And this is where autoimmune issues can start to show up. This is also where allergies can start to really go haywire. And so it’s a bad business.
And then lastly, the pH balance in your stomach is critical. One of the biggest misnomers in the acid reflux base is if you ask anybody on the street, why do you have acid reflux? They’re gonna say, because I have too much acid. Doctors say this. And it’s intuitive because we’re handing out acid-suppressing medications, but it’s entirely wrong. The acid in your stomach is critical for digestion in the base case. And unfortunately, we’re throwing a digestive-suppressive medicine at the problem where digestion is the problem.
But not only that, when you’re a soon of these too low, things like the bacteria that you swallow through your mouth are no longer encountered with that acidity and they’re able to grow in ways that they wouldn’t normally. It causes your immune system to have to go into overdrive. It can allow things like biofilms to grow. So we’re all familiar with things like plaque on your teeth. It’s when the bacteria create a protective housing so they can happily do their business without being brushed off. Well, for one, you’re swallowing those same bacteria in your stomach, but now you have no protection against that. But other bacteria can create biofilms as well. Some bacteria even create their own beneficial acidic environment. So that they can thrive without having to worry about a highly acidic environment to damage them. So all this stuff is going on, but we just thought we’re lowering acidity in order to reduce the acid in the throat. So you can start to see where there’s a really big problem here.
SIBO
I actually put a sixth item here. So I talked about the five curious things you need to know about to heal your acid reflux. There’s actually a sixth one. I’m not much of a specialist in this area. There’s a small intestinal bacterial overgrowth or SIBO, if you’ve probably heard that term, or IBS, irritable bowel syndrome. And this happens when you’ve got bacteria in your small intestine.
And the challenge there is unlike the large intestine or the colon, where when the bacteria break in foods down and they create gas that comes out through the posterior, you’re now in this little windy area of your small intestine, and there’s just nowhere for the gas to go. Your pyloric sphincter, which sits on top of it, is closed, and you’re in this windy area.
And so it’s excruciatingly painful to have these big gas bubbles forming. You know, I could talk to you a little bit about some symptom mitigation, because we’ve got some in our family. One of the things that you can do is you can lay on your side and allow the gas bubble to travel up. A lot of people that have IBS can say they can feel the gas bubble.
They turn to your side, allow it to travel up, and recognize that your body is doing this with the small intestine. Now you turn on the other side and allow it to go up. This is a much faster way to allow the bubble to pass. But really, what you need to be able to do is to get those bacteria that are in the wrong place out. And I can’t advise you on how to do that, because I haven’t really done a lot of research on it, but I thought I’d throw that in there, because a lot of people that deal with acid reflux also deal with IBS or SIBO because of the fact that they’re acidity in their stomach is compromised, and this allows things that would normally have gotten burned off through as the pyloric sphincter allows food contents to go into the small intestines. So you can see where, again, you start to develop problems and things that are seemingly unconnected are connected.
“Taking Pepcid and omeprazole, and I still feel like I have gas in my chest”.
So thanks, Amia, thanks for the comment there. Yeah, in fact, again, I’m not a doctor, but I’ll just give you my comments on this. Pepcid, which is an acid, one of the ones that I reached for early on, and I’ll just tell you, frankly, it’s probably the reason that I ended up getting on the medications in the first place because of the cycle that I just talked about. But Pepcid and ameprazole are acid reducers, and what that is doing is making it much more difficult for your body to digest the food that’s in your stomach.
So it sits there longer and allows for much more gas production than normally would have happened, and you’re gonna have a lot more gas as a result. So to fix the digestive issue, doctors are giving you digestion suppression medicines, which is just inherently wrong. I don’t get it, but that’s what they do. It’s no place we can go back and view the video later. Yes, there’s actually several places. So I think this will be posted on Instagram. That’s the one I’m not 100% sure of. It will be on my YouTube channel, and it will also be syndicated to podcasts. It will be available on every major podcast player. So you can go back and listen to it. There’ll also be a link to the show notes, so if there are any links or things that I talk about, you’ll be able to get those as well.
Healthy Stomach Acid pH
What’s your stomach pH be? So your stomach pH should be somewhere between, I believe, two and three. And I’ve heard, in some cases, maybe even as low as one, but that seems pretty significant. Just for reference, I think a car battery is one, so it’s really acidic. And the stomach acid that you have is actually hydrochloric acid, and so you may remember from school, hydrochloric acid is one of the most potent acids that’s out there. And for good reason, it’s breaking down your food into little biological components that can then be reconstructed to create you. So you kind of want that to work well.
Acid Rebound
“So once your symptoms approve, should you drop down to a less omeprazole?”
You know, if you go through the approach that I talk about in my book, what I would do, and what worked really well for me, is try to create a baseline on your diet to a point where you can start to have a sense for what’s going on trigger-wise and try to avoid things like triggers that may make the next phases of the program less challenging. There’s a lot more, I’m simplifying this, but that’s essentially what you’re trying to do. For me, I started taking a handful of supplements, and when I started taking those, I discontinued all the PPIs immediately.
I mean, the reason for that is they’re gonna counteract each other. And again, things like the omeprazole, with the acid suppression, they’re really doing you more harm than they’re doing good if you can safely get off of them. Now, you probably have experienced what I experienced. So when I was on acid reflux suppressing medications, I started on 10 milligrams.
My second doctor was like, “Okay, so you’ve got acid reflux, what are you doing for it?” It was like, “I’m taking PPIs.” And they were like, “Well, how long have you “been taking that?” It was like, “Seven years.” She was like, “You can’t take that stuff “for longer than six weeks.” I was like, “I know.” And then she doubled my dose. But the thing, and I kind of lost my train here. Oh yeah, so the thing that you’re gonna run into if you just stop taking it without support is acid rebound, to where you just don’t have a way to mitigate the challenges that you had that caused you to take the acid reflux medication in the first place. The underlying issues have not been solved.
And so you need some support through a protocol or things that I’ve talked about, like in my book. On my website, lots of resources and videos and things that can help you kind of go through that. It’s much more comprehensive than I can kind of talk about in an answer to a question.
Vas Cornel:
“Thank you for sharing your knowledge “and experiences, you’ve completely changed “my husband’s life.”
That’s so exciting. To me, this is one of the things that keeps me going. Sometimes it can be very frustrating. You try to pour a lot of information into people and they cherry pick it, “I’ll do this, I’ll do that, “I’ll do this,” and they’re like, “Well, why isn’t it working?” Your program doesn’t work. It’s like, well, you can’t cherry pick and expect good results, but I live for things like you’ve shared here and being able to hear that people have been able to change their lives. Having dealt with this for 15 years, particularly on the latter ends of it,
I couldn’t do anything without thinking about by symptoms. I mean, some of the stuff that was in the red in the chart that I showed you before, that’s all about the social stuff. Like I couldn’t even be around people without constantly being in fear of the anxiety that I had as a result of my reflux. At the time, I didn’t know it was related to my reflux, but I couldn’t even enjoy their company. I was just struggling all the time, so I get it. So being able to hear that someone’s had a breakthrough, like that’s what this is all about.
Yeah, so it’s a craft crush. I apologize, I was on a break, a pretty extended break. I was doing a lot of travel with my family, and I didn’t get to a lot of stuff, so feel free to send your email again, and I’ll try to get to it. But just being full disclosure, I get a tremendous amount of email and direct messages, and so I’ll try to get to it when I can. If I don’t get to it timely, please forgive me. I try to help, but the best way I can help is prevent more resources like this out there that people can kind of consume, and do a little bit of self-help as well.
How to close the Lower Esophageal Sphincter
I’m sorry to hear that, Kerry, that you’re feeling a lot worse. You’re on and I’m back to normal, so hopefully that means you’re moving in a good direction. A lazy sphincter, a placebo, and anxiety. That’s a lot going on. You know, with the lazy sphincter, it’s really all gonna be about kind of getting some of the stuff that’s lower in the body here back in gear, and let me explain why that is.
So in addition to making sure that you’re hormone production is back in place, and your enteric nervous system is running correctly, all that needs to be sort of functioning in concert in order for your sphincter to close properly. So inflamed or not, if you don’t have the right hormones, because they’re not being produced by your microbiome, your enteric nervous system literally cannot cause your sphincter to work in a responsive way, nor can it cause it to fully close.
And so that therein lies the challenge. Okay, I’m gonna come back to the comments here in just a second. So just the last little piece here with the colon, I talked a little bit about the bacterial balance, talked about the hormones, and I guess it really kind of covered everything on this particular slide. Let me know if you’ve got other questions on that that I really didn’t hit, but I’ll continue through the comments and questions that are there.
So just coming back to one of the points that was raised earlier. So things like the Heidelberg test are really helpful to be able to determine whether you’ve got low acidity, or you’ve got high acidity that you’re dealing with. I’ll tell you that if you’re a reflex upper, I would be completely shocked if you’re dealing with high acidity, not just because it’s a super rare case, this condition called hyperchlorhydria, but because there’s nutrient deficiencies, many of us are taking the medications, there’s bacteria that can produce a low acid environment. There’s so many reasons why you have low acidity and not high acidity, but the Heidelberg test can confirm it. Some people just need to know before they take any further steps. So that’s there if you can find a doctor that will make it available for you.
Microbiome Test
I do need to talk about the microbiome test. So it is not the silver bullet that we would hope that it is. It’s continuing to advance. So over the last 20 to 25 years, it’s been recognized that the body is not just a machine. There’s this whole other complex system of trillions of microbes that participate with the body, with hormone production, with inflammation reduction, actually even with immune function, that if it’s not working properly, things sort of start to cascade out of control. A entire study was commissioned called the Human Microbiome Project, where healthy donors provided their microbiome. And this is all the bacteria, fungi, viruses, protozoa, things that exist in the body.
They provided samples, and they’re able to use those samples and study them to understand and classify all the different species that exist in the hopes that you’d be able to figure out what’s the ideal configuration. How much of these beneficial strains do we need? How much of those ones do we need? How much commensal, how much?
And so they’re able to get a lot of stuff done, but it’s not perfect for a few different reasons. Some bacteria completely decompose outside of the human body.
Some, they’re just, we don’t know enough about it in order to put the right diagnostics in place in order to figure out what strains exist. There’s been almost no mapping of all the fungi, and we know it plays an important role as well. Synthesizing some of these bacteria again in the lab to create probiotics is not perfect. So, you know, I can go on and on about all the problems with the microbiome science that lead to imperfect probiotics. In addition, you know, the testing for the different strains is not perfect. And so all I’m getting at is it’s a great tool, and it can give you a very strong directional sense of where you may have issues. And for the known strains and for the easily testable strains, it can tell you you’re deficient and give you some real recommendations. It will not make you perfect. It will never restore you 100% because all the strains don’t exist. It can’t test for all of it. But it can help you like move in a big direction if you’ve got, you know, systemic or significant issues in the microbiome space. So it’s a bit of a disclaimer. I will put a link to the microbiome test that I recommend in the show notes. You can check that out as well. If you’re just not getting the breakthrough that you’re looking for, that may be, you know, something that could help kind of get things moving again.
So got a lot of great comments. For me, this is also just key. I’ve learned a ton that helped me heal my reflux. I’ve been able to see really positive messages like the ones that were shared where hundreds and hundreds of people will be able to successfully go through my program and be healed. Others have not. It’s hard for me to tell sitting in an armchair whether it was followed fully or they have other underlying issues that make it difficult.
So it’s just full disclosure. It may help you. It may leave some stuff that you still have to kind of figure out, including some of the things that we talked about today that aren’t incorporated yet into my book. But I think there is a tremendous opportunity here with this community of well over 10,000 people to share our experiences and things that have worked for us.
I will happily, you know, serve as a research engine to start looking some of this stuff up, codifying it together. But I think we can together really accelerate our journey towards healing. Maybe even more so than the resources I’ve already made available. So I’m super excited for that. That’s also why I’m excited about some of these comments. So apologies for the soapbox.
So Chris Chetti, I hope I pronounced that correctly. I’m happy that you were able to talk about some of the low stomach acid. I’m just curious about that. Hopefully I answered all your questions.
You also took the stomach acid test today through a naturopathic doctor and the result was low stomach acid. So that’s great that you’re able to get a hold of that test. Now I’m really curious though, was it a pH test in the throat or was it actually the Heidelberg test, the one that I talked about? Because it was hard to get a hold of. And if you got it, man, you’ve got a great doctor. Hold on to that one.
Feel like you've done all the things and are just not seeing progress? I've helped a lot of people over the years that felt the same way. Perhaps an at home microbiome test can help break the cycle and provide the insights you need to move froward. With it, you can test your gut microbiome and receive actionable recommendations on how to optimize your digestive health with the BIOHM Gut Report.
I have arranged a 20% discount if you use the code THEACIDREFLUXGUY at checkout!
Acupuncture for Acid Reflux
So Linda talks about, has anybody had any luck with acupuncture? So guys, please chime in. You know, I don’t have personal experience with acupuncture. I do see it quite often in the realm of things that are being clinically studied. I do spend a lot of time reading through medical journals and things like that. As I mentioned, I grew up in a medical household. Spent 40 years hearing table talk about a lot of these terms. I have a electrical engineering degree, so I’m not scared off by really technical materials. I read through a lot of it and that is what helped me develop my protocol to help myself, but it’s also provided people confidence that what I’m recommending is based on science. So I say all that to say that I do see acupuncture in the list of things that are kind of reviewed in literature for potential effectiveness. I have not read through a lot of those materials, so maybe some personal experience from you all would be helpful.
So John is making the connection here between stress levels and reflux. There is a direct correlation between stress levels and reflux. So one of the hormones that is produced by your microbiome. I think this one may be directly produced or may be converted, I can’t remember, but serotonin. It’s one of many sort of mood modulating hormones. And without serotonin, it’s hard. I spent a lot of years with severe apathy, depression, in addition to all the other stuff that I kind of flashed up on that slide. And there is hope as you begin to heal yourself. And I’m now on the three years on the other side of this thing.
A lot of that stuff has melted away. There’s still some residual. You can’t go through a lot of that stuff for 15 years and still have some residual stuff that you kind of deal with personally. But man, my mood is great. Keep pushing, keep doing positive things in the right direction. And I am very hopeful for you that you will get there.
Has anyone gotten gout?
I haven’t researched gout directly, but I can tell you that is one of those diseases that’s related to kind of the food that you’re ingesting. I have no doubt that it’s related to some of the gut health issues as well.
And Gabby even mentioned that there’s a higher prevalence of it with acid reflux. And so you start to see those connections again with gut health issues being an underlying problem and these different expressions of traditionally named diseases that probably are more symptoms than they are named diseases. So thanks for bringing that up.
And if anybody knows about correlation between gout and reflux, do please bring that up. And guys, if you’re on the replay later on, you can also add your comments to that as well. And we can all mine a lot of these comments for help. I will mine it for things I need to additionally research and create materials for you all. And you guys can mine it to help each other improve.
Okay, it was the Heidelberg. So thank you for confirming that. So it’s great to have that confirmation of what you’re dealing with because then you have that confidence moving forward that this is something that I can tackle. It’s a lot of what I hoped for and some of the diagnostics that the doctors would give us, but it’s just not there as we kind of covered before. Okay, so I’m gonna go back through this last round of comments and questions from Instagram.
I may repeat some of these again. I haven’t really honed my skills on live streaming yet, but we’ll get there. Also, Craft Crush, Ass Rebound is what happened to me. Really literally felt like it was burning in the back. Went up to PPIs two weeks ago. I really wanna get off of them. Yeah, pour through some of the materials that I share on my YouTube channel.
Reach out to me and kind of help talk you through some of these things as well and hopefully get you moving in the right direction. Exercise, now that’s a really great point, Amy’s music. Exercise, helping to get the gut moving. There’s this whole concept of motility, which I very briefly touched on. The esophageal manometry test starts to look at motility, which is the movement of food through your gastrointestinal tract. It starts as high as your throat. It’s these little bitty muscles that start to move things down.
You know, your lower esophageal sphincter can close, but it will even kind of massage and make sure things aren’t stuck in the folds and start to make sure the food gets moved down. That occurs all the way down your digestive tract.
Exercise is the best way to cause your digestive system to do that. So if you’ve got any sort of motility issues going on, if you’ve got reflux, you do have motility issues. You know, I’ve even heard that with small intestinal bacterial overgrowth, CBU or IBS, exercise can help with that as well because it causes those muscles to move and it might start to cause some of those bacteria that are in the wrong place to move on. So guys, exercise is absolutely key.
Thank you for the kind words, guys. I appreciate it. I’m glad that I’m able to help you all having suffered like I did. I know I don’t have all the answers, but man, I’m committed to try to get them and you guys can help me too as we kind of build this community together.
Yeah, absolutely. Curly note, anxiety as we talked about is directly related. I’ve got a video on my channel that talks about those links too, which can help you. You know, once you have that confirmation and you start to have some hope that you can latch on to and start to move forward in a positive direction. Finneigirl, yes, this is recorded. It will be available on YouTube and Instagram, I believe, but you can also go to the show notes or go to any of the major podcast apps and you will find it there as well.
Acid Reflux, Anxiety and Stress
Yes, I thought anxiety from stress. You know, I spent, and I shared this in my book and I’ll flash this up for you all just so you can see what my book is. This is only for the folks that are on YouTube, unfortunately I can’t do it on Instagram at the moment, but I was unaware for 15 years of the link between acid reflux and stress. At the same time that I got on PPIs, I got married, got a brand new job that had a whole lot more responsibility and I thought that some of the things that I was starting to feel were just related to me not really coping with this new situation very well.
I had no idea that the PPIs and the acid reflux disease itself were causing this suppression of things like serotonin, which are helpful for maintaining a positive mood. What’s the other dopamine? Maybe I’m gonna get myself in trouble. I can’t remember some of the other hormones. There’s another one that’s responsible for sort of the get up and go that causes you to kind of get after things that you think are important.
All these things go down when your microbiome is no longer producing them at the clip that it should be. But man, my anxiety went from just being a little bit nervous to being an absolute social wreck to the point where I couldn’t even be around people and enjoy them because I was so stressed and I had cognitive issues, I was having difficulty concentrating. I couldn’t follow the plot line in movies. I had to lean in like this when someone was talking to me just to kind of keep the thread of conversation in my mind. And with that sort of concentration issues and my social anxiety, I just knew I was gonna say something stupid and that stressed me out. I mean, it was just, anybody that’s dealing with that still, I’m sorry, and I know how you feel.
Can you Heal Reflux with a Hiatal Hernia
What about when you have a hiatal hernia? So I have a hiatal hernia. I told you I went to get an E.G.D. They confirmed two things with that. An E.G.D., if you’re not familiar with it, is a scope with a little camera on it that put it through your mouth, down into your stomach and do a visual inspection. So as they passed through my lower esophageal sphincter, they could see that I have a high-level hernia.
And then they just told me, you’re gonna have reflux for life, which I remember two car rides home from doctor’s appointments. Of all the doctor’s appointments I’ve had for all different things, I remember two and they’re both reflux. It was my very first one. And I remember this one because I thought, I don’t know if I can deal with this for the rest of my life. Just being perfectly frank. And with that diagnosis by high-level hernia and confirmation from my E.N.T. that I’ll always have it.
But I still have a high-level hernia. And I’ll tell you why I know that. So now I have no reflux symptoms whatsoever. I eat what I want. I’m still careful to make sure that I’m being healthy overall.
Only time I actually do have a little bit of reflux is, and I’m noticing this now because I’ve been doing a lot of travel here recently, is if I try to sleep on a plane. So I’m a tall guy. I can never find a good comfortable position. I’m six foot two. My head tilts down when I try to sleep or to the side. And with my high-level hernia, I think, with it being sort of deformed because of the hernia, tilting my head in that direction causes a misalignment which allows just a little bit of reflux out. And so I wake up in any plane ride where I successfully sleep with some stuff I got to spit out. But other than that, I have no reflux whatsoever. And so there is hope if you have a high-level hernia. Another confirmation of this for me when I was researching this for the very first time, you know, I was starting to find stuff like, give me hope, maybe I can do some natural things to deal with this. But then I thought, no, high-level hernia. The ENT said I’m gonna have it for life and it’s a structural deformity. Like, what am I gonna do about that?
I found that 50% of people over the age of 60 have a high-level hernia. And the vast majority of them don’t necessarily have acid reflux. And so two pieces of data that can help you realize that it is possible. Can I say everybody with a high-level hernia will be able to be healed? No, because I don’t know, you know, there’s probably some really big ones, there’s some really significant ones. I just, there’s no research. The other challenge I deal with is there’s a sort of a worldview that exists that acid reflux is caused by high acidity. And a compromised a lower esophageal sphincter, which they typically will say is because he lifted weight or something like that and it caused it.
So with that worldview, that takes all of the clinical studies, not all of them, but a lot of them. And so it’s difficult to research things like, what is the nature of a high-level hernia that would be too difficult to overcome? Like, I can’t research that as much as I’ve tried, because I want to give you guys numbers. So some of you will say, well, I’ve got a two centimeter high-level hernia, can I heal with that? I don’t know, because I can’t prove it. I would love to get enough of us together to where we can kind of pull that information together at some point in the future and be able to answer that question, but I can’t, unfortunately.
Should I get Hiatal Hernia Surgery
A coworker has done it and they don’t have any gastro problems anymore.
So two comments on that. I almost did it. And this was very early on in my reflex journey. This is a case where one of the doctors for real that flux actually saved me. He said, don’t do it, because there’s not been enough advances in the science yet. I’ve seen way too many relapses, excuse me, after the surgery. And you’ll find yourself down the line with a surgical procedure and the underlying issues never having been resolved. And it just undoes itself, or causes other complications. There’s people that end up with permanent burping fits so they can’t stop like every minute of the day. Some really severe and bizarre complications that can occur with this. If you think about everything we covered before, and if you came in late, think about all the issues and that are related to acid reflux. If you just put a band-aid on your high-level hernia without resolving the other issues,
it’s gonna become overcome like the high-level hernia was overcome in the first place to get you the reflux. It’s just a matter of time. And so I personally would rather try to deal with underlying issues and see if that resolves it completely, than try to stitch closed or put a medical device or a series of magnets or any of that sort of stuff that’s been invented because it’s not resolving the actual underlying issue.
Now, I have also read a lot of studies about the Nissin Fundoplication, which is one of the leading surgical procedures that are out there right now. Unfortunately, there is a pretty good track record early on, but after two, three, five, 10, 15 years, you start potentially getting some pretty bad complications as a result of it, again, because the underlying issues weren’t solved.
So, I’d encourage you the best you can try not to look for the quick fix, and I’m not suggesting you’re doing that. I appreciate you sharing the information that your co-workers had a good result from it, and I hope that they do well.
Try to figure out how you can resolve the underlying issues, chase that as hard as you can, and then if you don’t get any relief from that, I can understand where you may want to try something else. Carolina, I’m waiting for a miracle for you as well. A lot of times it takes a incredibly high degree of diligence, patience, persistence, and continuing to do one thing that improves your situation after another, and sometimes it can take time. You’ve seen several people mention on the call here that they’re able to successfully resolve the reflux after many, many years of dealing with it. And so, leverage the community, leverage me to help in the resources that we provide if you can.
Does DGL Work for Acid Reflux
DGL, so that’s actually one of those supplements that I would absolutely love to research if you guys are interested in it. So, I’m gonna let you guys kind of drive what videos I’m creating next, because I’ve seen some cursory information that indicates that DGL is absolutely what it says it is in terms of helping with inflammation in the stomach. Welcome for all the recommendations, and you guys are sharing with each other in the chat. This is amazing, so thank you for doing that.
PPIs Make Acid Reflux Worse
Yeah, trying to come off those medications is really, really difficult without the right support. You know, I’m with you on taking medications. I’m probably super extreme, and maybe to an unhealthy level at this point, with my apprehension of taking any medication. So, coming from where I’m coming from, I spent 15 years taking those PPIs under the illusion that they were helping me. And I would be okay if they weren’t helping me, if they were just keeping me stable, but they made me worse, and not just a little bit worse, they made me significant worse, not for other issues. I realized other medications have other side effects. They made the issue that they were trying to resolve significantly worse, and I’ve got a real big problem with that. I know that these doctors, and they’re doing their best, I’m not trying to throw shade at them, are seeing the same patients come back with the same issues that are not resolved or even worse.
And they’re still prescribing this stuff. I know they’re trying to help, but you gotta have some courage. As a doctor, I could not do that. I would say, look, I’m not in the position to help you. I’m not gonna give you these medications, because I’ve seen in my practice that it makes people worse. Or it’s not preventing them from getting worse.
COVID and Acid Reflux
COVID is another one of those complications that has caused people to either develop or to extend the reflex symptoms. I am Lauren, thank you for mentioning that. It’s not something I’ve talked about in a public forum yet, but just like antibiotics, COVID is another one of those where people have been reaching out, and it’s been the catalyst for them.
How long did it take you to get off the PPIs?
For me, it was a solid two months. The videos I got on my YouTube channel kind of talked through one of the supplements, was Betaine HCl, in addition to a comprehensive approach that helped me to get off the supplements. I’m really comfortable in a lot of these videos now, and even on my blog, because initially I was super excited to get information out there. I put things like all the supplements and stuff that I used.
But then people try to take it and cherry pick it, and they don’t do everything. And then they run into trouble. And so I’ve tried to be a little bit more strategic in how I package this information up so that you’re seeing the entire thing. And then if you choose to do the wrong thing, it’s up to you, and we’re all kind of free to make our own choices. But I want to try to help people be successful, is the deal.
Heart doctor told you it wasn’t stress, it was your heart, it’s the acid. Diagnosed the chronic gastritis, small hiatal hernia, and acid reflux.
I was actually chatting with somebody yesterday, and I pulled up my own EGD report, and I had missed that I have a little bit of gastritis was identified. Some of you have my book, I put the copy of my EGG report in there, but you can see, there’s some gastritis, I didn’t even see that. So I didn’t realize I had a little bit of that going on.
Severe reflux for 12 years. So Murphy, you bring up a really good point. Another thing that I’m really frustrated with, a lot of these diagnostics results, design tests about. A lot of these, in the best case, they’re kind of confirming you have reflux, but you already knew, I mean, reflux is one of those super easy self-diagnosis type things. But in the worst case, doctors are sending people home saying you don’t have anything wrong with you. If nothing comes up in the test, you’re fine. When you’re not.
Hiatal Hernias
Yeah, I hear you Finney on the endoscopy. Sometimes, you know, the other, some people ask me a lot of times, did I get a follow-up EGG? Because in my book, I talk about the fact that they found polyps, which are these little bumpy protrusions that occur because you’ve taken the PPI medications for so long. The problem with them is over time, they can become cancerous. They did a biopsy, no cancer was found, that’s now been like 11 years. I never did a follow. So I hope and I pray that I don’t have any cancer, but I don’t know, I’ve never done a follow-up. And I completely understand what you’re saying about being nervous about what they find. The other thing is I felt like my reflux was worse right after.
Now I don’t know if that was because of the stress of hearing that I had a hiatal hernia, or if that was because of, you know, sort of the invasive procedure of sticking an implement down through my esophageal sphincter. I don’t know, and I haven’t seen any results on that.
The doctor told me I was born with one.
There’s a lot of bad information going on around hiatal hernias. Now, to be honest, I have not been able to locate some research that gives definitive information about what creates a hiatal hernia. My doctor told me it was from lifting weights, which made sense to me at the time. I mean, you straighten yourself, you can call us hernias. But how is the ring muscle on your throat connected to anything over here?
It’s not. It doesn’t really make any sense. I think more likely, and again, I can’t prove this, this is just conjecture. Many of you probably have hemorrhoids. This is sort of a canary in the coal mine. When you’re having issues dealing with inflammation, we don’t have some of the anti-inflammatory properties that come from a healthy microbiome. One of the very first places is the place right next to your colon, and you’re gonna start to have some of the anal sphincter, which is another type of sphincter, like the one you’re through. It’s gonna start to push out.
I have a theory that the esophageal sphincter can behave in the same way, where it can actually cause a little bit of a deformation when you’re dealing with some of those inflammation issues. Can’t prove it, I don’t know if it’s true. That’s just a theory of mine. Because I wonder if that participated in the success that I’ve seen despite the fact that I have a hiatal hernia. I have some of the inflammation reduced and was able to allow closure.
I was gonna ask about the esophageal sphincter. Mine is causing swallowing issues. One of the things that you can do, it’s difficult if you’re unable to get a quick handle on some of the reflex issues that are causing inflammation on the esopahgeal sphincter. One of the things that’s in your control is reducing the amount of acidic foods that you ingest.
A very little bit of acidic food, like an apple or a banana, which you might think is pretty benign, but is actually pretty acidic. If you’re dealing with inflammation issues in that area, we’ll inflame it further and reduce the closing pressure. I put together a course that I talk about what to eat. One of the things I have on there is a column full of all the foods and their pH levels. That can be a guide, but you can also Google a lot of this stuff. Make sure you’re looking for the pH level of the fruit, not the pH level of the soil that the fruit is put in. Similar thing with the vegetables.
But avoid foods that are above, or I should say below, between one and five pH, like the plague. That’s all your acidic foods. These are all your packaged foods. Your canned foods, a lot of fruits, not all of them. These things are gonna cause additional challenges.
Overeating and Acid Reflux
Over-eating because of anxiety. You know, it’s great that you can kind of say that out loud. It’s important to be able to recognize those things. You can start to work towards them. You know, overeating is gonna create additional pressure on your stomach. It’s gonna lead to additional bloating. It’s gonna lead to additional indigestion issues. You probably have anxiety while you’re doing it. The hard thing about digestion, particularly when you have anxiety, is your body really needs to be in a parasympathetic state, which is a relaxed state, in order to digest properly. When you’re in stress or in anxiety, your digestion suffers greatly. And it just contributes to the overall cycle. So I used to run off and grab a lot of fast food, eat on the go while I’m trying to get to my next meeting or whatever, I had to cut that out. I had to plan it in advance. I had to make sure that I was being calm when I was eating, in addition to chewing fully. I mean, there’s all these things that you wanna do that I talk about in my book together because no one thing is gonna help you break down this complexity.
But recognizing that is really the first step towards it. You’ve got it. You just work at it.
I only did the one is endoscopy, and you probably asked that a little bit earlier. I hope you guys are learning a lot of good information here. I realize I’m kinda going a little bit long. I appreciate you sticking around for your patience to be with me here. I’m gonna try to do these every week. And on Instagram, if you follow me there, I’m gonna ask you what you would like for the next subject to be. I’ve got a bunch of ideas of things I think would have been official to you, but I wanna allow you to drive that. And we can have an information session, some of the one that I just did, but also go through a Q&A where I can help you try to think through some of the things that you may be challenging with.
You can tell from all the stuff that we talked about, this is a complex issue, but you wanna continue to get this stuff in your brain so that you’re able to kinda think through it and really help yourself. It requires a lot of sort of internal detective work, diligence, patience, continuing to make things a little bit better. Let me give you one big power tip.
Anytime you’ve got any sort of friction in terms of something that you’re trying to do new, it can be really difficult. If it’s a little bit easier to do the old thing, a lot of times you may do it. One of the things that my wife really helped me with early on is we recognized things like sugar, or like the worst possible thing that I could eat when I’m trying to heal with my reflux, as we went through and removed all the stuff that was in our pantry that had background sugars. So I’m not talking about getting really cake batter or cookies or any of that kind of stuff. I wasn’t gonna eat that because I’ve committed to working towards my healing. And I know that a step back on things like sugar causes viral explosion of the pathogenic bacteria and sets you really back, right? So it’s not just a, I’m gonna bear through this little trigger incident.
It’s really setting yourself back. So I was committed. So she got rid of all the background sugar. And what I mean by that is, if you flip your bread bag over and look at the label, you’ll see it’s got added sugars. And this is refined sugar. This is the stuff that’s really bad for you. You look at your ketchup label, it’s got refined sugars. Everything, particularly in the Western diet has added sugars. And this is absolutely detrimental to healing. You’ve got to get rid of that stuff. You will not see progress. I’m not talking about not eating sugar in the future. I’m talking about getting yourself square, getting yourself healed, never cheating while you’re working on this to the best extent you can.
Get yourself right, and then you move on with the rest of your life. I’m back to where I can enjoy ice cream. I couldn’t even look at a glass of milk because of my reflex issues, kind of related to some of the allergy challenges that I talked about. But I got my gut health right, and I’m back in business, right? So do yourself a favor, be committed, be diligent, and work through it. I know that you can do it.
So guys, we’ve talked through a lot today. We’ve talked about each of the five areas of the body that you need to be knowledgeable about, and I hope this will allow you to have a more informed discussion with your doctor, but also to really be able to test all the different things that are out there in terms of try this for acid reflux. Don’t do this for acid reflux. You should hopefully have, and if you need to go back through it and watch the replay, a foundational knowledge to say, you’re recommending that, but it does not address any of these key areas in a way that makes sense. So you’re not being blown around with all these different remedies. And that’s what I want for you, is I want you to have a solid knowledge of these things so that you can move confidently in a good direction, whether you use the approach I used or you use another one.
Next week, we will talk about some of the healthy foods, the label, healthy foods. This is, again, another situation where people are kind of pushing at you, what’s healthy. But is it, though, for your reflux? And we’re gonna talk through that. So if you’re here on the replay, you can just click on the video, but otherwise, we will catch you next week and I appreciate your attention. Guys, have a great day and take care of the rest of your healing journey.

Medical Disclaimer: The content of this site is for informational purposes only, and to give you ideas for you and your physician to research. It is not intended as individualized advice to treat, cure, mitigate or prevent any medical condition.
Disclosure: This is a free website so I do advertise to cover the costs of website hosting and other services. If you find the information on this site useful, please consider making a purchase using the following links as I will earn a small commission at no cost to you.
Connect With Me
 Take advantage of my daily tips on Instagram, YouTube, or join my mailing list to learn how hundreds, just like you, have taken control of their health!
Take advantage of my daily tips on Instagram, YouTube, or join my mailing list to learn how hundreds, just like you, have taken control of their health!
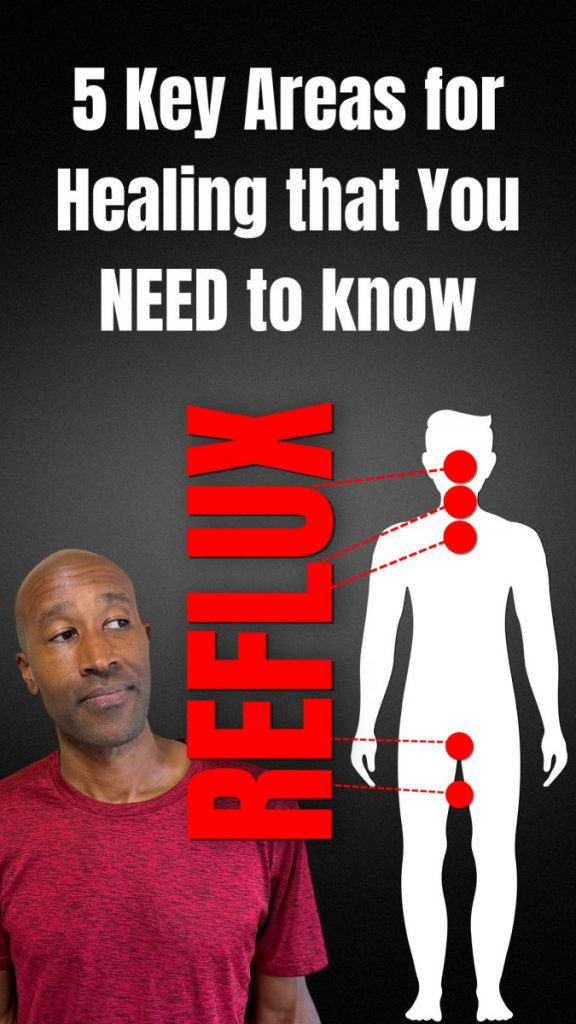
Don Daniels
Latest posts by Don Daniels (see all)
- The Purple Lie We’ve All Been Sold. Proof Inside - December 22, 2023
- I Had Reflux for 15 Years. Here’s What I Learned - December 15, 2023
- 5 At Home Low Stomach Acid Tests for Reflux - September 11, 2023



Hi Don, Do you do paid consultations ever? I am struggling with an acid reflux problem, and eating probiotic foods definitely helps a lot, so I’m getting your book and I’m going to try your program & stop my PPI. I’m very hopeful it will help since drinking kefir every day has already helped so much. However, I still have a question that I’d love to discuss with you that I don’t see on your website, and it has to do with potential overstrain of the LES from intense exercise (this is just my personal theory, I don’t know if… Read more »
Hi Anna, I try and provide free resources that will answer common questions. In this way I can help more people, but I do have individual conversations from time to time. Let me email you to see how I can best help.
Best Regards,
Don